Context: Retrospective data thus far has supported improved responses with HMA/venetoclax combinations in both the frontline and relapsed settings. A Phase Ib trial of azacitidine and venetoclax for high-risk MDS patients demonstrated an overall response rate (ORR) of 80%. Retrospective data from the Moffitt Centre comparing HMA/venetoclax to patients who received HMA showed an ORR of 77% compared to 40% for patients who only received HMA.
Objectives: Our aim was to obtain real-world evidence for use of combination HMA/venetoclax to treat myelodysplastic patients in the Arabian Gulf region.
Methods: This is a retrospective study of patients with myelodysplastic neoplasm treated with a HMA/venetoclax in 4 different countries from Jan 2020 - May 2023. Cases were included if they were over the age of 18, and had a diagnosis of MDS or MDS/AML. Both frontline and relapsed/refractory patients were included. Patients were excluded if they had more than 20% blasts or received an additional agent with their treatment.
Results: Data on 16 patients was collected across 4 centres in the Arabian Gulf. The median age was 66 (range 51-84). All patients had high-risk MDS, MDS/AML including four patients with a TP53 mutation and/or complex cytogenetics. Median follow-up was 15 months (range 4-23). A median of 6 cycles were received (range 3-14). Azacitidine was the only HMA used at a starting dose of 75mg/m 2 for 7 days. Venetoclax starting dose was 400mg (or equivalent if given with an azole) and given for a median of 15 days (range 10-28). Thirteen patients received azole prophylaxis. Thirteen patients achieved a CR/CRi (81%), one patient who didn't had a TP53 mutation with complex cytogenetics, another had secondary MDS, and the third had stable disease and proceeded to transplant.
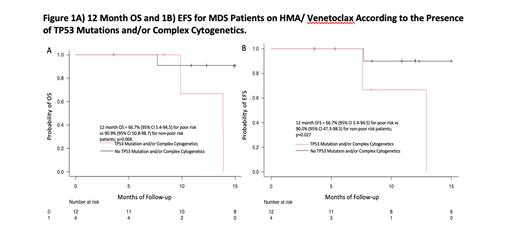
Overall survival (OS) at 12 months was 86.2% (95% CI 55.0-96.4). For patients with poor risk disease (TP53 or complex cytogenetics) OS was 66.7% (95% CI 5.4-94.5) vs 90.9% (95% CI 50.8-98.7) for non-poor risk patients; p=0.006. Median OS was 22 months (22-NR) for non-poor risk patients compared to 14 months (10-NR) for poor risk patients. Event-free survival (failure, transformation or relapse) at 12 months was 84.6% (95% CI 51.2-95.9); it was 90.0% (95% CI 47.3-98.5) for those with no poor risk features and 66.7% (5.4-94.5) for those with poor-risk features; p=0.027. For those who stopped, 4/16 stopped due to failure and disease progression or transformation, 4/16 underwent stem cell transplantation, 3 stopped due to infectious complications, two from drug access issues, and one patient with secondary MDS had recurrence of their primary solid tumour. The most common toxicities were cytopenias and one patient died from cellulitis and COVID while on HMA/venetoclax.
Conclusion: The combination of HMA/ venetoclax is a feasible treatment for patients with high-risk MDS with significantly worse outcomes in patients with complex cytogenetics and/or TP53 mutations. This regimen seems to be adapted by many hematologists in our region. However, the long-term efficacy in comparison to standard of care for various subgroups of MDS needs to be explored in larger prospective studies
OffLabel Disclosure:
No relevant conflicts of interest to declare.
Azacitidine and Venetoclax for MDS

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal